Let’s sum up the situation on the widespread lack of understanding and contempt towards food intolerances and allergies. We have heard just about anything and everything on the subject, and that's not only from the mouth of patients, but doctors too.
First let me set forth a few definitions. The word “intolerance” means the absence of a reaction by the immune system. In contrast, use of the term “allergy” implies an immune system reaction through the intermediaries of one of its two great actions: cellular immunity (via the white blood cells, that is to say the neutrophils or the lymphocytes) and humoral immunity (via the antibodies also called immunoglobulins).
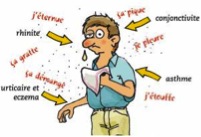
Immunoglobulins are divided into several categories and the ones we are interested in here are IgE, IgG and IgA. IgE allergies are characterized by immediate reactions, which are potentially severe (the most extreme manifestation being anaphylactic shock). It represents 'classic' food allergy, with symptoms affecting the gastrointestinal tract (such as cramps, diarrhea, vomiting), the skin (such as hives, itching, eczema), and respiratory symptoms (such as asthma and laryngeal edema). In severe cases (anaphylactic shock), multiple organs are involved, wherein severe hypotension, along with respiratory and cardiovascular distress, can be life threatening. IgE antibodies can be detected in the blood or in sub-cutaneous tests called skin prick tests. Generally speaking, these reactions generate flagrant symptoms, most of the time.
 IgA allergies correspond to a precise pathology, namely coeliac disease (severe allergy to gluten: multiple proteins from diverse cereals such as wheat, rye, barley and oat). This condition entails profound perturbations of the intestinal mucosa with hyper-permeability (leaky gut) and malabsorption. Anybody interested can learn a lot more via my website www.gmouton.com under the banners “articles” (references 7a, 7c & 7f) and “conferences” (see section Nutrition and Function).
IgA allergies correspond to a precise pathology, namely coeliac disease (severe allergy to gluten: multiple proteins from diverse cereals such as wheat, rye, barley and oat). This condition entails profound perturbations of the intestinal mucosa with hyper-permeability (leaky gut) and malabsorption. Anybody interested can learn a lot more via my website www.gmouton.com under the banners “articles” (references 7a, 7c & 7f) and “conferences” (see section Nutrition and Function).
IgG allergies reflect delayed immune reactions, seldom generating obvious clinical symptoms following immediate food intake. They therefore remain unknown to the patient except if we are looking for them through a blood test (important: request quantitative tests and not qualitative). In this case, detection is not possible via a skin test, as with the IgE antibodies.
 IgG allergies are often called food “hyper-sensitivity” to distinguish them clearly from classic IgE allergies. This terminology doesn’t bother me at all, even if these are a form of true allergy, producing IgG antibodies. The more inspired specialists call them “non-IgE allergies” which reflects the complexity of immune reactions involved, furthermore involving, partially, cellular immunity.
IgG allergies are often called food “hyper-sensitivity” to distinguish them clearly from classic IgE allergies. This terminology doesn’t bother me at all, even if these are a form of true allergy, producing IgG antibodies. The more inspired specialists call them “non-IgE allergies” which reflects the complexity of immune reactions involved, furthermore involving, partially, cellular immunity.
On the other hand, calling IgG allergies “intolerances” is inappropriate because it is the source of severe confusion. By definition, intolerances represent adverse reactions to some foods without the involvement of the immune system. The best example is lactose intolerance, characterized by the absence of the enzyme capable of digesting this disaccharide, namely lactase. This doesn’t involve the immune system at all, as is the case also with (at least with our current comprehension) sulfites or monosodium glutamate (MSG), two other well-known causes of intolerance. When this intolerance involves lactose or fructose, the detection is only possible through a breath test and not through a blood test, nor a skin test. Confusion of this kind doesn’t help the patient to see clearly, making careful adherence to the definitions a must!





